#1 AI Voice Agent for Healthcare
AI Voice Agents
for Patient Access and RCM
Tailor-made to handle patient, provider, and payor calls, so your team can focus on care


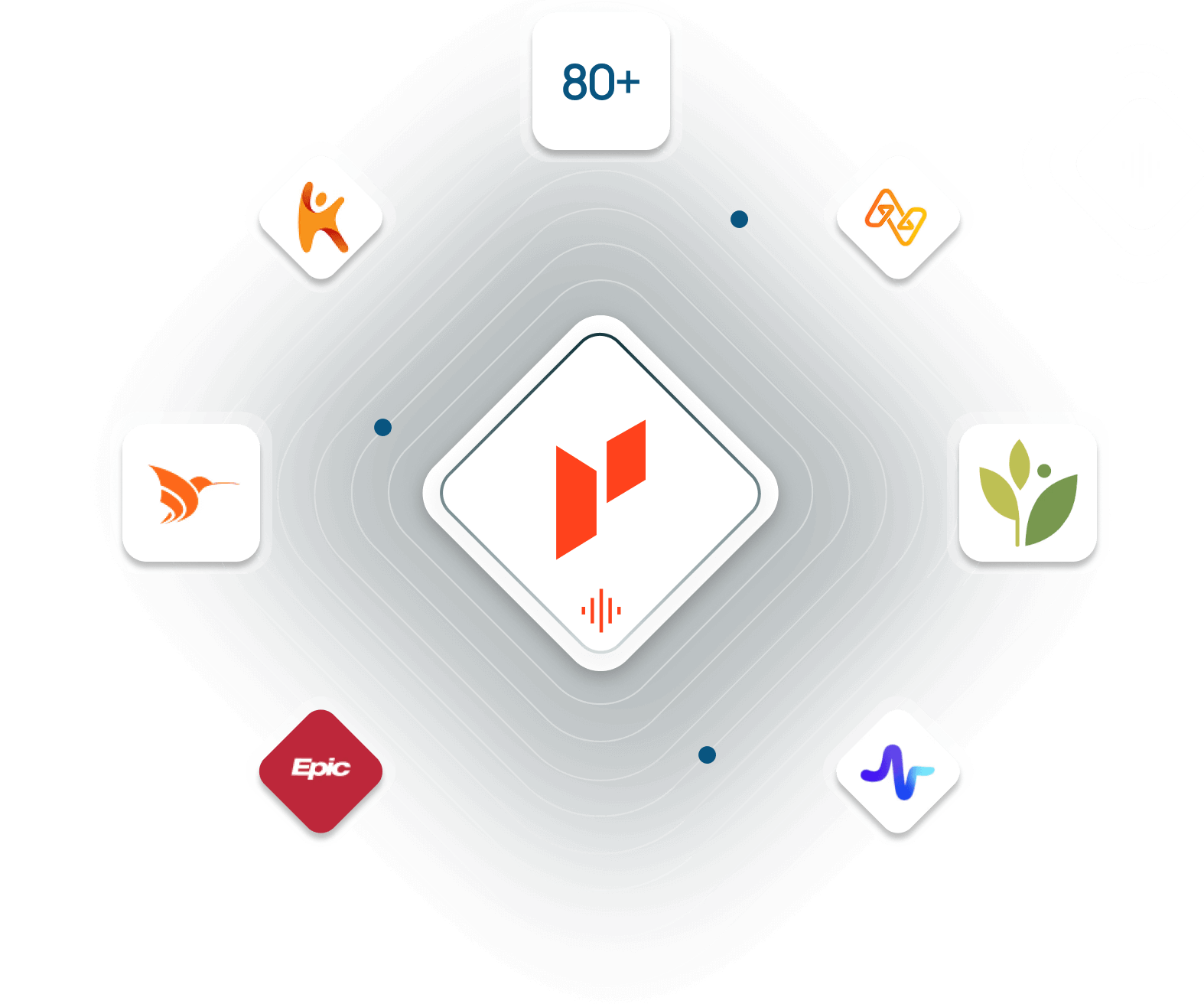
Switchboard

Appointment Scheduling

Benefit Verification

Patient Billing
Annual Re-Engagement



+80 integrations